After Nearly 14-Year Battle with Both Breast and Thyroid Cancer, Former Jackson Memorial Mammogram Technician Fights Lymphedema with Help from Specialized Therapy at Jackson North
After Nearly 14-Year Battle with Both Breast and Thyroid Cancer, Former Jackson Memorial Mammogram Technician Fights Lymphedema with Help from Specialized Therapy at Jackson North







Tamera Johnson, 49, knows what it means to fight hard. As a former radiology and mammogram technician at the Roberta Orlen Chaplin Digital Breast Imaging Center/Taylor Breast Health Center at Jackson Memorial Hospital, she saw breast cancer patients and survivors every day.
“I saw everything – from women who came and passed away, to women who came back and were cancer-free,” Johnson said. “I never imagined I would become a patient, too.”
In December 2010, Johnson felt a knot in her left breast when she reached over for the television remote control at home.
“I remember that I sat up immediately in my bed and felt it,” Johnson said. “I always found it strange when patients reported knots showed up ‘out of nowhere’ – until it happened to me the same exact way.”
On December 23, 2010, a biopsy revealed that Johnson had breast cancer.
She was only 36 at the time.
For the next 10 years, she did everything she could to fight the disease, including a double mastectomy, a total hysterectomy, removal of her ovaries, and removal of her lymph nodes underneath her left arm. Additionally, she underwent chemotherapy and radiation for a year after her surgeries.
“I just knew that I wanted to fight because I didn’t want to die,” Johnson said. “The chemotherapy felt like someone was pulling every piece of energy out of your body. If I wanted to live, I had to fight with all that I had. It was a strength I never would have imagined I had.”
In January 2012, Johnson finished chemo and radiation therapies, and was cancer-free. She then underwent breast reconstruction surgery, which involved a lengthy waiting period due to skin damage from radiation therapy.
That same year, Johnson’s doctor suspected she also had thyroid cancer. Rather than take chances, she followed her oncologist’s recommendation and had a total thyroidectomy.
In 2022, after years of taking chemotherapy medication and remaining in remission, Johnson’s oncologist informed her that she was cured and again cancer-free.
“Although you never feel like yourself again, I feel blessed that I’m still here,” Johnson said.
For her entire cancer battle, she also suffered from lymphedema, a condition where fluid builds up in the body, usually in the arms or legs, causing swelling.
Over the years, Johnson received lymphedema therapy and did at-home exercises. However, the swelling became more uncomfortable, and in 2024, she was referred to Jackson North Medical Center for treatment, where she met Erica Poulin, an occupational therapist and certified lymphedema specialist.
“When Tamera came to me, her left arm was weak and felt heavy for her, making it hard for her to carry groceries and put on clothes. She was also feeling self-conscious with the way it looked,” Poulin said. “The swelling was impacting her quality of life and affecting her ability to fully participate in her roles.”
For a month, Johnson and Poulin worked on specific grip-strength exercises, and developed plans to help significantly reduce the swelling, including bandaging the arm, massages, compressions, and exercise.
“When it comes to lymphedema, we empower our patients to become independent with managing it at home. We practice exercises, compression, and massage until the swelling is reduced to fit the patient for a sleeve and maintain our results,” Poulin said. “It’s so important to know and understand what lymphedema is and how to treat it, because you’d be surprised how many patients come to us after major surgeries and have never heard of it before.”
Following lymphedema therapy at Jackson North, Johnson saw improvements in her arm’s range of motion, strength, and size. She regained the ability to wrap her arm independently, wear lymphedema sleeves comfortably, dress herself, and feel confident again.
“Tamera did so wonderful, and she was really excited about the improvements she saw – she was feeling a lot better,” Poulin said.
Today, Johnson remains cancer-free, thanks to annual visits with both her oncologist and lymphedema specialist. She focuses on managing her lymphedema and swelling, advocating for more breast cancer education in the African-American community, and maintaining a healthy lifestyle through diet and exercise.
“After so many years of battling cancer, my advice to any cancer patient is to fight – fight with all you have,” Johnson said. “Don’t give up – stay strong, and surround yourself with family and friends – don’t worry about anything else, because you will get through it.”
Jackson Saves Local Businessman and Entrepreneur, Paul Flanigan
Jackson Saves Local Businessman and Entrepreneur, Paul Flanigan





By: Miranda Torres
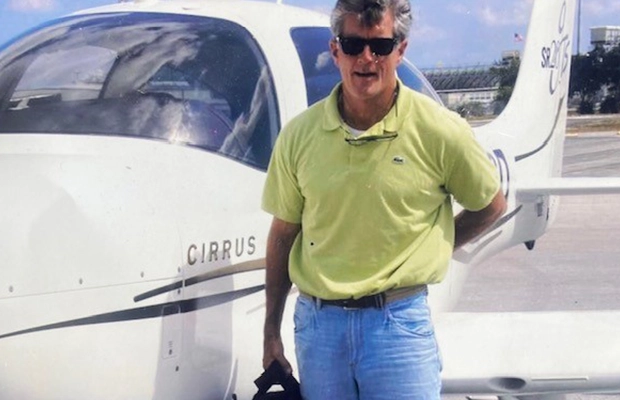
Paul Flanigan, 67, experienced a life-altering event when the plane he was piloting crashed on a golf course in Key Largo on March 1, 2024. He was airlifted to Ryder Trauma Center at Jackson South, which was just the beginning of his journey with Jackson Health System.
Flanigan, a well-respected local entrepreneur, has long been intertwined with the community, including a successful decade-long partnership with Flanigan’s Enterprises Inc., where he managed several of the beloved Flanigan’s Seafood Bar and Grill franchises. Later, he purchased Quarterdeck from Flanigan’s Enterprises, and established multiple locations across Florida.
Flanigan arrived at Ryder Trauma with severe fractures to his hip and knee area. He was cared for by Joyce Kaufman, MD, a critical care surgeon, and Marilyn Heng, MD, an orthopedic trauma surgeon. Dr. Heng operated on his hip. Two days later, Flanigan underwent surgery to address the fracture around his knee.
The plane crash came just four years after a bicycle accident caused Flanigan to break part of his pelvis, which triggered severe arthritis. The injuries he sustained during the plane crash caused his arthritis to accelerate, leaving him with discomfort and a limited range of motion. Flanigan eventually had a total hip replacement with Dr. Heng.
“Every step of the way during my time at Jackson, it seemed like there was help there instantaneously,” he said. “My previous crash meant I sort of knew what to expect, but I was grateful for how knowledgeable and friendly they were, especially since I didn’t know how long I would be there. I was blessed.”
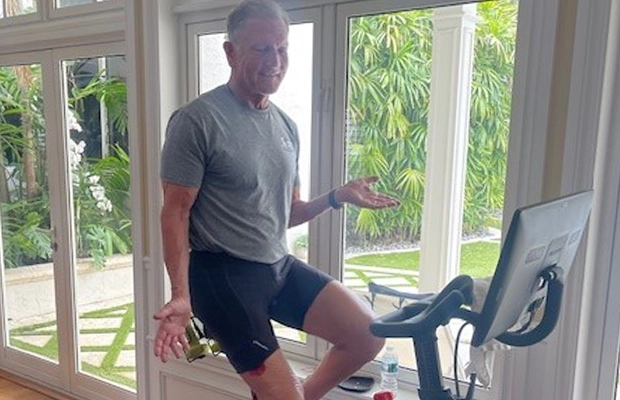
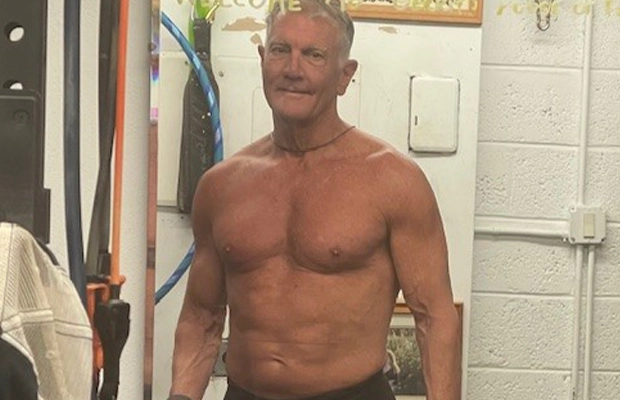
Since his hip replacement, Flanigan has been receiving physical therapy to help him regain his total range of motion. He was non-weight bearing for the first 10 weeks of his rehabilitation, but is now getting back to the activities he loves most, like playing pickleball, chasing after his grandchildren, and dancing with his wife, Michelle.
“For his age, he’s fantastically active and very kind in terms of always being polite and good natured. His love of activity and function is of a much younger person,” Dr. Heng said.
While Flanigan’s recovery is well underway, another challenge awaits: a knee replacement surgery with Victor Hernandez, MD, an orthopedic surgeon with UHealth – University of Miami Health System. Flanigan remains optimistic and is eager to regain full mobility so he can focus on what matters most to him—his family.
“I could never thank the team at Jackson enough,” Flanigan said. “If I could, I’d share the blessings I receive at the conclusion of every mass: ‘May the almighty God bless you and keep you safe to love and serve others.’”
St. Croix couple involved in hit and run recovers with help from Ryder Trauma Center and Lynn Rehabilitation Center
St. Croix couple involved in hit and run recovers with help from Ryder Trauma Center and Lynn Rehabilitation Center







By: Krysten Brenlla
Kevin Stalbaum, 63, and his wife, Amy Stalbaum, 53, live for adventure. After Kevin worked for the U.S. Air Force and Arizona’s Power and Water Company for years, the couple decided a quiet retirement awaited them in the Caribbean island of St. Croix.
“The scuba diving in St. Croix is amazing. We’re renovating our hurricane-damaged dream house on the island ourselves, and there is a great cycling community there,” Amy said. “Cycling is one of our favorite things to do together.”
They never thought the activity they loved the most would almost cost them their lives.
On September 17, the Stalbaums began their bike ride at 6:45 a.m. Less than 10 minutes into their ride, a car crashed into both of them from behind.
“We’re both experienced cyclists, and we do everything we can to be as visible and as safe as possible,” Amy said. “Despite our precautions, we were hit, and we don’t know why. The driver and the car are still missing.”
The impact from the crash left both Amy and Kevin unconscious on the road. Emergency medical services arrived to the scene and rushed the couple to the nearest emergency room on the island, where doctors diagnosed Kevin with leg, cervical, and lumbar fractures, and Amy with severe road rash, a brain bleed, and a spinal fracture.
“At one point, I remember being on a gurney, with Amy on her gurney next to me,” Kevin said. “I remember asking, ‘what’s going on?’ And that’s the last thing I remember before waking up in Miami.”
Because of the severity of their injuries, Amy and Kevin needed to be medically evacuated to the nearest trauma center, and by Monday, September 18, the Stalbaums arrived to Ryder Trauma Center at Jackson Memorial by helicopter, where they were prepped for emergency surgery.
“The first thing we had to do with Kevin was make sure he was stabilized from a cardio pulmonary standpoint,” said Stephen Shelby Burks, Jr., MD, a UHealth – University of Miami Health System neurosurgeon and spinal cord surgeon at Jackson. “He needed a collar due to his cervical fracture, and a custom lumbar brace. For Kevin’s lumbar surgery, we used a CT-based navigation surgical system, which enabled us to direct the screws in the exact position needed. With this procedure, we hope to mitigate Kevin’s pain, and avoid any deformities in his spine from forming in the future.”
At the same time, Amy was also undergoing spinal surgery.
“The ligaments of Amy’s spine were ripped apart,” said Evan J. Trapana, MD, a UHealth orthopedic spine surgeon at Jackson. “Amy is very young and active, which is why we went the route we did by placing rods and screws in her spine to stiffen the spine’s structure, giving her a stable construct for her body to weigh on. In six months, when everything is healed up, we’ll remove the rods and screws to preserve most of her motion and lower the risk of her needing future spinal surgery.”
Amy’s surgical team used robot-assisted surgery to place the screws and rods in her spine; Jackson Memorial is one of a few hospitals in the nation with the robot technology available for use in spinal surgery.
“It really helps us, as surgeons, safely implement screws with pinpoint accuracy,” Dr. Trapana said. “It also shaves time in the operation, and provides a better recovery rate for patients.”
After spending nearly three weeks in the hospital, the Stalbaums were discharged on October 10. They received rehabilitation therapy at Christine E. Lynn Rehabilitation Center for The Miami Project to Cure Paralysis at UHealth/Jackson Memorial, and created comprehensive plans with therapists to help with their mobility, balance, endurance, and strength.
With the help of physical, occupational, and cognitive therapies, the couple look forward to making a full recovery, so they can return to St. Croix.
They’re grateful to the teams at Ryder Trauma and Jackson Memorial for not only saving their lives, but giving them the chance to keep their adventures going for years to come.
“We count our blessings that we landed here,” Amy said. “Jackson’s staff and our community back home in St. Croix really helped us get through this.”
St. Croix Doctor Who Suffers Heart Attack Is Airlifted to Miami for a Lifesaving Surgery by Jackson Cardiac Team
St. Croix Doctor Who Suffers Heart Attack Is Airlifted to Miami for a Lifesaving Surgery by Jackson Cardiac Team


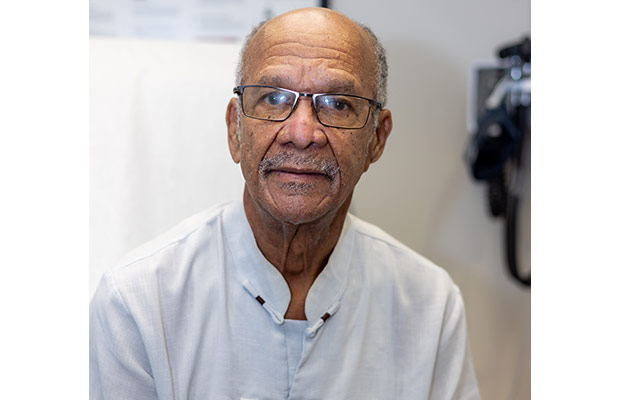

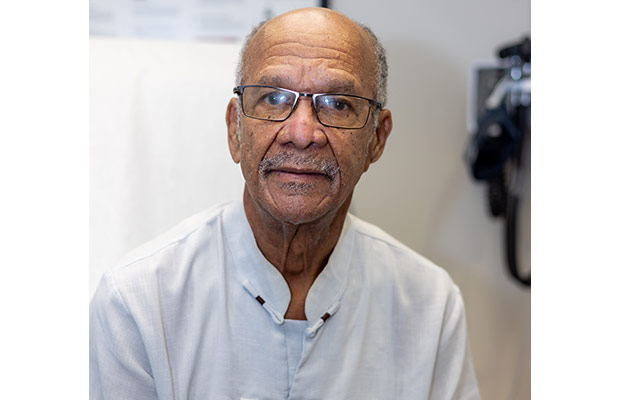
Lloyd Henry, MD, has spent decades saving lives as a general surgeon at Governor Juan F. Luis Hospital in St. Croix, U.S. Virgin Islands. At age 84, he had lived a healthy life with no prior medical concerns. However, that changed on November 16, 2021.
While assisting in an open gallbladder removal surgery, Dr. Henry suddenly began to experience fainting episodes. Fainting, also known as syncopal episodes, results from a sudden drop in heart rate and blood pressure. It is often due to strain, stress, or long periods of standing, all of which Dr. Henry experienced.
“We were finishing up and I just felt strange,” he recalled. “I looked at the other surgeon and told him that I felt funny.”
The next thing Dr. Henry remembers was waking up in the operating room with severe right lower back pain, numbness, and difficulty moving his right foot. Upon evaluation, the medical team revealed the situation was much more serious. He would need medical attention at a facility with the expertise and resources to give him the best care.
The next day, Dr. Henry was airlifted to Jackson Memorial Hospital.
Jackson Memorial’s cardiothoracic medical team immediately performed an echocardiogram and a computed tomography angiography (CTA) of his chest and abdomen that revealed a tear in his aorta, also known as the coronary artery – the artery that delivers oxygenated blood from the heart to the rest of the body. According to the National Library of Medicine, less than 50 percent of patients with a ruptured aorta survive. Exams also revealed that there were signs of mild-to-moderate aortic valve regurgitation, which is a condition that occurs when the heart’s aortic valve does not close tightly.
The team called in the expertise of Romualdo Segurola, MD, Jackson Health System’s chief of cardiac surgery and director of the Jackson Heart Institute.
“The most impressive thing about Jackson to me is that it’s the only true comprehensive health system in South Florida. Our advanced technology also sets us apart,” Dr. Segurola said. “The teams that treated Dr. Henry involved cardiothoracic surgery, cardiology, and critical care. Together, they were able to see to all his needs in a timely and effective way.”
Dr. Segurola performed multiple surgeries on Dr. Henry, including an emergency ascending aortic dissection repair, aortic valve replacement, and an exclusion amputation of the left atrial appendage that helps prevent strokes by sealing off a small section of the heart called the left atrial appendage. This is a site where blood clots may form during an arrhythmic episode.
All the procedures were successful. Dr. Henry was able to return home to St. Croix within two weeks and was back at work two months later. Today, in addition to his work at the hospital in St. Croix, he takes pride in his gardening, time with his wife, and seeing his seven grandchildren and five great-grandchildren grow up.
“Jackson is like the major leagues. The staff is excellent from beginning to end,” Dr. Henry said. “I owe my healthy track record to my faith, taking care of myself, and giving back to my community, but I thank the top medical care I was able to access that has given me my life back.”
Baby Born with Congenital Heart Disease Receives Treatment at Holtz Children’s Hospital
Baby Born with Congenital Heart Disease Receives Treatment at Holtz Children’s Hospital



Lloyd Henry, MD, has spent decades saving lives as a general surgeon at Governor Juan F. Luis Hospital in St. Croix, U.S. Virgin Islands. At age 84, he had lived a healthy life with no prior medical concerns. However, that changed on November 16, 2021.
While assisting in an open gallbladder removal surgery, Dr. Henry suddenly began to experience fainting episodes. Fainting, also known as syncopal episodes, results from a sudden drop in heart rate and blood pressure. It is often due to strain, stress, or long periods of standing, all of which Dr. Henry experienced.
“We were finishing up and I just felt strange,” he recalled. “I looked at the other surgeon and told him that I felt funny.”
The next thing Dr. Henry remembers was waking up in the operating room with severe right lower back pain, numbness, and difficulty moving his right foot. Upon evaluation, the medical team revealed the situation was much more serious. He would need medical attention at a facility with the expertise and resources to give him the best care.
The next day, Dr. Henry was airlifted to Jackson Memorial Hospital.
Jackson Memorial’s cardiothoracic medical team immediately performed an echocardiogram and a computed tomography angiography (CTA) of his chest and abdomen that revealed a tear in his aorta, also known as the coronary artery – the artery that delivers oxygenated blood from the heart to the rest of the body. According to the National Library of Medicine, less than 50 percent of patients with a ruptured aorta survive. Exams also revealed that there were signs of mild-to-moderate aortic valve regurgitation, which is a condition that occurs when the heart’s aortic valve does not close tightly.
The team called in the expertise of Romualdo Segurola, MD, Jackson Health System’s chief of cardiac surgery and director of the Jackson Heart Institute.
“The most impressive thing about Jackson to me is that it’s the only true comprehensive health system in South Florida. Our advanced technology also sets us apart,” Dr. Segurola said. “The teams that treated Dr. Henry involved cardiothoracic surgery, cardiology, and critical care. Together, they were able to see to all his needs in a timely and effective way.”
Dr. Segurola performed multiple surgeries on Dr. Henry, including an emergency ascending aortic dissection repair, aortic valve replacement, and an exclusion amputation of the left atrial appendage that helps prevent strokes by sealing off a small section of the heart called the left atrial appendage. This is a site where blood clots may form during an arrhythmic episode.
All the procedures were successful. Dr. Henry was able to return home to St. Croix within two weeks and was back at work two months later. Today, in addition to his work at the hospital in St. Croix, he takes pride in his gardening, time with his wife, and seeing his seven grandchildren and five great-grandchildren grow up.
“Jackson is like the major leagues. The staff is excellent from beginning to end,” Dr. Henry said. “I owe my healthy track record to my faith, taking care of myself, and giving back to my community, but I thank the top medical care I was able to access that has given me my life back.”
$16 Million Grant Provided by Shriners Children’s Hospital
$16 Million Grant Provided by Shriners Children’s Hospital



Lloyd Henry, MD, has spent decades saving lives as a general surgeon at Governor Juan F. Luis Hospital in St. Croix, U.S. Virgin Islands. At age 84, he had lived a healthy life with no prior medical concerns. However, that changed on November 16, 2021.
While assisting in an open gallbladder removal surgery, Dr. Henry suddenly began to experience fainting episodes. Fainting, also known as syncopal episodes, results from a sudden drop in heart rate and blood pressure. It is often due to strain, stress, or long periods of standing, all of which Dr. Henry experienced.
“We were finishing up and I just felt strange,” he recalled. “I looked at the other surgeon and told him that I felt funny.”
The next thing Dr. Henry remembers was waking up in the operating room with severe right lower back pain, numbness, and difficulty moving his right foot. Upon evaluation, the medical team revealed the situation was much more serious. He would need medical attention at a facility with the expertise and resources to give him the best care.
The next day, Dr. Henry was airlifted to Jackson Memorial Hospital.
Jackson Memorial’s cardiothoracic medical team immediately performed an echocardiogram and a computed tomography angiography (CTA) of his chest and abdomen that revealed a tear in his aorta, also known as the coronary artery – the artery that delivers oxygenated blood from the heart to the rest of the body. According to the National Library of Medicine, less than 50 percent of patients with a ruptured aorta survive. Exams also revealed that there were signs of mild-to-moderate aortic valve regurgitation, which is a condition that occurs when the heart’s aortic valve does not close tightly.
The team called in the expertise of Romualdo Segurola, MD, Jackson Health System’s chief of cardiac surgery and director of the Jackson Heart Institute.
“The most impressive thing about Jackson to me is that it’s the only true comprehensive health system in South Florida. Our advanced technology also sets us apart,” Dr. Segurola said. “The teams that treated Dr. Henry involved cardiothoracic surgery, cardiology, and critical care. Together, they were able to see to all his needs in a timely and effective way.”
Dr. Segurola performed multiple surgeries on Dr. Henry, including an emergency ascending aortic dissection repair, aortic valve replacement, and an exclusion amputation of the left atrial appendage that helps prevent strokes by sealing off a small section of the heart called the left atrial appendage. This is a site where blood clots may form during an arrhythmic episode.
All the procedures were successful. Dr. Henry was able to return home to St. Croix within two weeks and was back at work two months later. Today, in addition to his work at the hospital in St. Croix, he takes pride in his gardening, time with his wife, and seeing his seven grandchildren and five great-grandchildren grow up.
“Jackson is like the major leagues. The staff is excellent from beginning to end,” Dr. Henry said. “I owe my healthy track record to my faith, taking care of myself, and giving back to my community, but I thank the top medical care I was able to access that has given me my life back.”
Mom Looks Forward to Taking Baby Home After Preterm Birth
Mom Looks Forward to Taking Baby Home After Preterm Birth




When Latevia Ward, a third-grade teacher in Miami, went to the hospital in August at 27 weeks pregnant, she knew something wasn’t right. She was recovering from a recent bout of COVID-19 but felt like she was experiencing early signs of labor.
Doctors at the Women’s Hospital at Jackson Memorial Hospital were monitoring her closely because Ward — a mother of 7 — had a history of preterm labor and preeclampsia, which results in dangerously high blood pressure during pregnancy.
Just one year ago, on August 6th, 2020, Ward delivered twins at 27 weeks. The twins, Aidan and Asia, weighed less than two pounds and struggled with many complications. Ward lost both within a matter of months — one-month-old Aidan on Labor Day and four-month-old Asia on Thanksgiving morning.
In 2018, Ward lost another baby girl, Miracle, who was also born prematurely.
With this pregnancy, Ward had been in the hospital several times already due to issues stemming from preeclampsia, which was frustrating because she only had high blood pressure when pregnant. And after losing her previous three babies, she tried to get as healthy as possible.
“You can’t be prepared for it,” Ward said of preeclampsia. “[Before this pregnancy] I had lost weight, was eating right and everything, and wasn’t even on high blood pressure medicine. But as soon as I got pregnant, preeclampsia came back.”
Ward continued to go to the hospital every three days for monitoring. Then, doctors checked her cervix and realized she was dilated, a sign her body was preparing for labor.
Ward was in the hospital on bed rest for seven days, and doctors gave her medications to try to slow or stop the delivery and to prevent complications in the baby if it was born early.
On September 14, Ward went into labor and delivered a baby boy via cesarean section. Aaron weighed 4 pounds. The moment Ward heard him cry, she knew something was different. She never heard her twins cry because as soon as they were born, they needed to be intubated to help them breathe.
“When I heard him cry, I started crying because it was a relief to me,” she said.
Aaron was whisked away to the Neonatal Intensive Care Unit (NICU) at Holtz Children’s Hospital, the largest Level III NICU in the region that can provide care for the sickest and smallest babies.
Within four days, Aaron was off the CPAP breathing machine, but Ward was still nervous. She feared something would go wrong.
“I was afraid about everything,” she said. “I was so sad all over again thinking about my other babies.”
The nurses in the NICU, especially those who know her from the previous year, have reassured her each day that Aaron is doing well and getting stronger. He is tolerating food and is learning to suck to be able to eat from a bottle. He is now 8 weeks old, weighing more than 5 pounds.
“He’s alert and doing better,” Ward said. “I’m able to relax a little. But I still have some bad days, [especially since] November is when I lost Asia.”
Despite her understandable fears after her unimaginable loss, Ward has faith that Aaron will pull through.
“You just have to stay strong. I’m spiritual, and I read my Bible to stay positive, and I have positive friends around me,” Ward said.
Ward’s original due date was November 25, and doctors believed he would be ready to go home by then, but on Friday, November 12, Ward received the much-awaited that her baby boy was finally coming home.
Ward is looking forward to that day.
“I’m thankful to God that my son has finally come home and now we get to spend time together as a family,” She said.
A Mother’s Unconditional Love Gives Son a Fighting Chance to Receive a Life-saving Kidney Transplant
A Mother’s Unconditional Love Gives Son a Fighting Chance to Receive a Life-saving Kidney Transplant





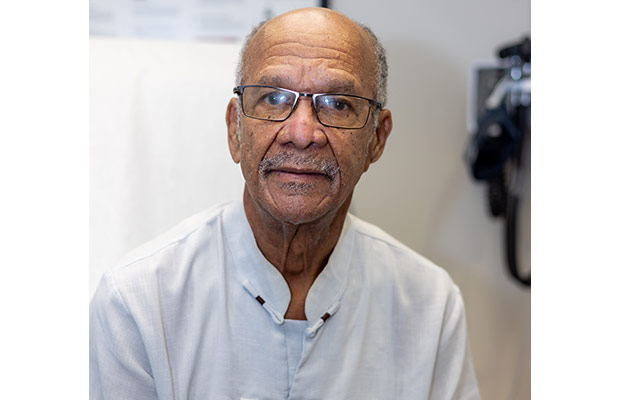
When Araceli Cantero Obregón was seven months pregnant, doctors in Nicaragua told her that her son Edgard Sequeira would have hydrocephalus, a condition in which excess cerebrospinal fluid (CSF) builds up within the ventricles of the brain. She was also advised that they identified spina bifida, which occurs when a baby’s spinal cord fails to develop properly in the womb.
Despite the heartbreaking news, Obregón was not going to give up on her first-born son, who she welcomed into the world on September 6, 2007. By the time Edgard turned one, he had undergone surgery for both conditions. The procedures allowed the family a sense of normalcy for a few years, but the young boy continued to face medical setbacks and personal hardships.
Throughout his childhood, Edgard was not developing physically or cognitively. He also was experiencing complications with his bladder and kidneys. Furthermore, Obregon began noticing her son was lacking energy. He was isolated from his friends and had occasional seizures.
In 2016, pediatricians in Nicaragua ran tests and gave Obregon frightening news — her son was diagnosed with chronic kidney disease (CKD) and would need to start dialysis immediately. Edgard was also suffering from high blood pressure. The diagnosis was an all too familiar red flag for Obregón, who had lost her husband to CKD two years prior.
“It was traumatic to hear my son was suffering from the same disease that took my husband,” Obregón said. “My whole world was falling apart.”
After years of attempts with no sustainable treatment, Obregón desperately sought the care of pediatric nephrologists at Holtz Children’s Hospital, leaving Nicaragua for the U.S. in February 2020.
When Edgard arrived at Holtz Children’s, he was malnourished, weighing 50 pounds at 12 years old. After a thorough examination, his team of nephrologists determined he needed intervention in urology, nutrition, and blood pressure care before he could be listed on the national transplant waiting list. He would also need to continue receiving dialysis four times a week while being monitored by the pediatric transplant team at the Miami Transplant Institute (MTI).
Due to the COVID-19 pandemic, the family was also faced with the decision of having to stay in Miami long-term. For Edgard to have a fighting chance, Obregón knew the best decision was to stay in South Florida and make sure her son completed his treatments.
Thanks to the help and financial support of family, friends, and Miami’s Corpus Christi Catholic Church, Edgar and Obregon were able to stay in the U.S. and continue with Edgar’s care.
Over time, Edgard, now 14, had breakthroughs in his health, and last October, he was listed on the national transplant list. Five days after her son was listed, Obregón received the call from MTI that they were ready to perform the life-saving procedure.
The successful kidney transplant was led by Mahmoud Morsi, MD, and a multidisciplinary team at Holtz Children’s.
“I am eternally grateful to everyone, the social workers, the nurses, the nephrologists, the Holtz team, the MTI team, and so many others who have become a part of our family,” Obregón said. “There is no way to repay them for giving my son a chance to have a better quality of life.”
For the care team, miracle stories like these also remind them of their life’s calling as medical professionals.
“It’s a gift for them, and it’s a gift for us,” said UHealth pediatric nephrologist Jayanthi Chandar, MD. “It gives us a sense of fulfillment and happiness to see our patients thrive and witness extraordinary changes in their mental, emotional, and physical state.”
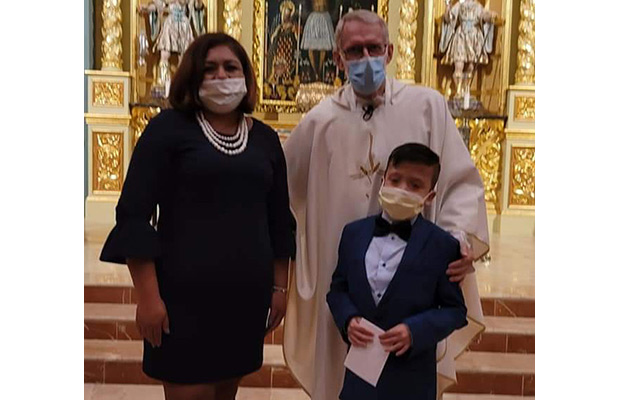
After 123 Days in the NICU, Baby is Reunited with his Parents
After 123 Days in the NICU, Baby is Reunited with his Parents


When Patricia Fusco and Katrina Wegmann were in high school, Patricia shared that she would not be able to carry and birth her own children. Unbeknownst to Patricia, Katrina decided then that if she was able to when the time came, she would be a surrogate for her friend.
Little did they know that more than 20 years later, not only would they still be close friends, but their husbands would also be best friends. And when Patricia and her husband, Andrew, had trouble finding a surrogate, Katrina stepped up.
Katrina, who already had two children of her own, expected it would be “another easy pregnancy and it would be able to make them a family.”
The pregnancy turned out to be anything but easy. Twelve weeks into her pregnancy, Katrina’s blood pressure was high — something she’d never experienced before, causing the pregnancy to be considered “high risk.”
Turning to Jackson for High-Risk Care
As the pregnancy progressed, Patricia, a senior specialist for community outreach and events at Jackson Health System, asked Katrina to consider meeting with the Maternal Fetal Medicine team at Jackson Health System. Every year at work, Patricia plans multiple events, including the NICU reunion, where babies who were saved and cared for at the Holtz Children’s Hospital Neonatal Intensive Care Unit (NICU) are reunited with their medical teams.
“I know that Jackson treats over 50 percent of South Florida’s high-risk pregnancies and that the Holtz Children’s Hospital NICU is one of the largest and best in the nation,” she said. “Working at Jackson, I hear the miracle stories all the time. But you never think you’re going to be one of those miracle stories.”
Katrina and Patricia immediately felt comfortable and confident in the Jackson team. They were followed by Jackson Medical Group physicians, Dana L. Homer III, MD, FACOG, an OB/GYN, and Felipe Tudela, MD, FACOG, an OB/GYN and maternal fetal medicine specialist.
Patricia called Tudela “a gift to his profession.”
“He’s probably the best doctor I have ever had the pleasure of meeting,” she said. “Everyone on the team invests themselves wholeheartedly in each patient’s case.”
When Katrina was 23 weeks pregnant, she suffered from terrible headaches, and her blood pressure was extremely high. She was admitted to the hospital and told she would need to remain there on bed rest to try to prevent an early delivery. That meant a possible two-to-three-month hospital stay – a stressful complication since she had two small children at home. Later they would confirm she had preeclampsia, a potentially dangerous pregnancy complication associated with high blood pressure.
A Difficult Choice
Two weeks later, a routine ultrasound showed that the baby was not growing and there was concern with the placenta, which was no longer providing critical nutrition to the baby. Dr. Tudela told them to consider delivering the baby early because he did not know if the baby would survive otherwise. Patricia, Katrina, and their husbands came together to make the difficult decision.
“That was a terrifying day for us, probably one of the most emotional days,” Patricia said. “Ultimately, we trusted the Jackson NICU enough that we preferred to deliver him then, rather than seeing what could happen if we tried to keep him in utero.”
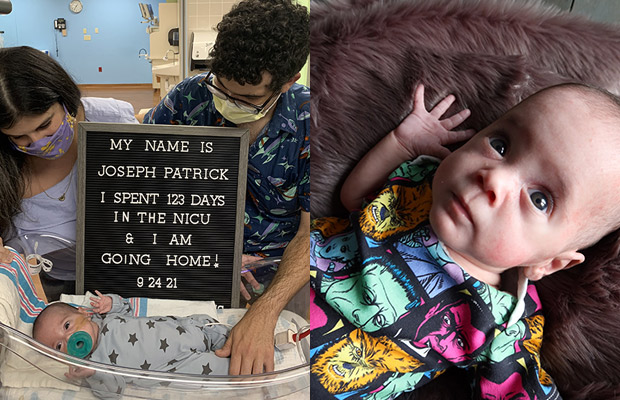
On May 27, 2021, at 25 weeks and five days gestation, Joseph Patrick, nicknamed JP, was born weighing just 1 pound 4 ounces. Quickly, doctors told the Fuscos that they made the right choice as there was no more amniotic fluid in the sac, and the baby would not likely have survived if they had waited.
As soon as the Fuscos saw their baby in the NICU, they felt more at ease.
“When we saw him, I thought, ‘they’ve got this,” Patricia said. “Once he was stable in the NICU, things began to feel safe. And every step of the way from that day forward, the doctors, nurses, therapists, everyone at every level always kept us abreast of what was going on.”
The NICU Village
JP thankfully had no brain bleeds and a fairly smooth ride in the NICU, with some breathing complications and an unknown infection during his stay. He remained in the NICU for 123 days.
“They say it takes a village [to care for a child], and I can wholeheartedly say there is no better village than the NICU village at Holtz Children’s,” Patricia said.
During JP’s stay, Patricia and Andrew said they were a part of every conversation regarding his care and the nurses became their friends, confidants, and teachers.
In addition to the expert and compassionate care that both Katrina and JP received, Patricia said she is grateful that everyone at Jackson treated their uncommon situation as if it were an everyday occurrence.
“We had a unique situation because we were high-risk. It was also unique because it was a surrogacy, and we were two friends going through this together,” Patricia said. “We know that our situation is not common. It definitely is not something they see every day. But every single physician, every single healthcare worker, never batted an eye at us. Everyone treated the experience with understanding and compassion. I don’t know if that would have been the case at another hospital.”
In September, after a nearly four-month NICU stay, JP was able to go home.
“It was a relief to finally be able to walk out of those doors with our son,” Patricia said. “It felt like an accomplishment.”
A Special Bond
JP continues to grow and thrive but is closely monitored by doctors and specialists to make sure he’s developing and that no more complications arise. Patricia and Andrew are now enjoying what they call a more “normal” stage of parenting.
“We’ve already seen him grow from a fragile 1-pound infant to a robust, beautiful baby boy,” Andrew said. “Now I’m looking forward to watching him hit those milestones, not only growth and developmental milestones but the little kid moments that define a childhood.”
And Katrina is happy that she will be there to witness it all. While they still need to be careful about visits due to the pandemic, the families are closer than ever.
“I talk to my kids about JP all the time, and they can’t wait to spend time with him. I look forward to them growing up together,” she said.
The experience “intertwined” the families forever, Patricia said.
“We are eternally grateful to her,” she said. “There are no words or ways we could ever adequately repay or thank her for what she has given us.”
Baby Reunites with Parents after Months in the NICU
Baby Reunites with Parents after Months in the NICU

In December 2020, Daniel Furlong, a former urology resident at Jackson Memorial Hospital, and his wife, Sarah, were packing for their babymoon trip – four months before the expected arrival of their first child – when suddenly, Sarah began to experience uterine cramps.
The couple immediately rushed to The Women’s Hospital at Jackson Memorial, where doctors determined Sarah was in preterm labor. She remained hospitalized for observation, but the baby just couldn’t wait.
On December 30, 2020, with the help of Rachel Franklyn, MD, Jackson Medical Group associate medical director of obstetrics and gynecology, Sarah gave birth to a baby boy at nearly 25 weeks. Ryder, who weighed just 1 pound, 10 ounces, was immediately rushed to the neonatal intensive care unit (NICU) at Holtz Children’s Hospital. He remained intubated in the NICU for two months and had to overcome several medical setbacks, including pneumonia and brain bleeds, which caused him to have several seizures.
Ryder was also diagnosed with a condition called patent ductus arteriosus (PDA), an opening between the two major blood vessels leading from the heart that normally closes shortly after birth. He underwent a PDA ligation procedure, performed by Eduardo Alfonso Perez, MD, a University of Miami Health System pediatric surgeon, to correct the birth defect.
“He had to overcome so many medical challenges in the NICU that his medical team began calling him ‘Ryder the fighter’,” his father, Dr. Furlong, recalled.
When Dr. Furlong wasn’t tending to his patients, he was at his son’s bedside. Due to COVID-19 visitation restrictions, he and his wife took turns visiting Ryder.
“As a physician, I struggled with knowing too much and trying to relay that information to my wife without scaring her while being honest with her about Ryder’s progress,” Dr. Furlong said.
Last May, after spending 125 days in the NICU, Ryder was finally able to go home. The Furlong’s family and friends had anxiously awaited for this moment to come.
“Having Ryder as a patient was a journey for my staff and me,” said Dianne Bennett, ARNP, director of patient care services at Holtz Children’s. “Seeing him finally reunited with his parents after all he had gone through was such a heartwarming moment.”
Dr. Furlong and his wife are happy to be settling in with their son.
“Hearing Ryder cry at home was such a relieving moment,” Dr. Furlong said. “My wife and I had waited months to finally be with our son. We were so overjoyed to have him with us.”
Ryder will continue to visit various specialists to make sure he’s progressing and meeting important developmental milestones.
“As a member of the Jackson family, it was encouraging to know that my son was truly in the best care possible,” Dr. Furlong said. “My wife and I are so appreciative and thankful to everyone who took care of Ryder, including all of the doctors, nurses, therapists, and ancillary staff who treated and loved him as their own child.”