A Birthday Miracle: A New Heart Gives One Florida Man A Second Chance at Life
A Birthday Miracle: A New Heart Gives One Florida Man A Second Chance at Life



Harold Jean never knew that he was born with a heart condition. He lived a normal childhood, played sports, and exercised. But in 2005, at the age of 23, he suffered a minor stroke.
He quickly recovered, but it was the beginning of a series of health problems. Ten years later, at age 33, Jean learned his heart was weak. He was diagnosed with congestive heart failure and needed a pacemaker to help control his heartbeat.
“Even with the pacemaker, I could run and exercise,” he said. “I used to ride my bike often and was part of the Brickell Run Club.”
However, that all changed on November 23, 2020.
“I was home alone when all of a sudden, I couldn’t breathe,” he recalled.
He immediately called for a ride to Jackson Memorial Hospital.
“When I arrived at the hospital, I fainted in the emergency department,” he said. “After I woke up, I was in a hospital bed. The doctors told me if I hadn’t made it to the hospital when I did, I would’ve died.”
Anita Phancao, MD, FACC, Chief of Heart Failure, Mechanical Circulatory Support, Transplant Cardiology at the Miami Transplant Institute, was one of the doctors treating Jean.
“When Harold arrived at the hospital, he was experiencing shortness of breath, and we quickly discovered he was in cardiogenic shock, which means his heart could not pump enough blood through his body,” Dr. Phancao said. “We started him on IV medication to help support his heart and put in a balloon pump and admitted him to the intensive care unit (ICU). He was very sick, and so we put in for expedited advanced cardiac therapy, including listing him for a heart transplant.”
Due to the ongoing COVID-19 pandemic, visitors weren’t allowed in the hospital, so Jean couldn’t have his family at his bedside. Luckily, the ICU nurses caring for him stepped in. They spent time talking with him and keeping his spirits up.
“I love my nurses,” he said. “They took incredible care of me and became my family in their absence. They were so important for my mental health.”
On his birthday, the nurses that Jean had begun to call family surprised him with a cake and a birthday celebration. Then came the greatest gift of all.
“My nurse surprised me with the news that I would be receiving a new heart,” Jean said. “I was so overwhelmed with emotion and began to cry.”
On December 14, 2020 – Jean’s 40th birthday – Jean underwent a successful heart transplant.
“Despite everything going on in the world with the pandemic, our transplant team has remained steadfast and committed to performing these lifesaving procedures,” said Matthias Loebe, MD, PhD, FCCP, FACC, Chief of Heart and Lung Transplant and Mechanical Support at Miami Transplant Institute, who performed Jean’s heart transplant.
After his transplant, Jean remained hospitalized, undergoing physical therapy at the Christine E. Lynn Rehabilitation Center for The Miami Project to Cure Paralysis at UHealth/Jackson Memorial for six months as he slowly recovered and learned to walk again.
“It was a difficult challenge, but I trusted the process,” he said. “By practicing my rehab exercises each day, I was finally able to walk. Jackson is truly the best hospital in the world. They did a great job, and now I’m back to living my life.”
For Jean’s medical team, seeing him thrive is the best gift.
“Our number one goal when performing a transplant,” Dr. Loebe said, “is to help our patients get better and well enough to go back to living their life.”
Today, Jean has resumed the activities he used to enjoy, such as exercising and running. And just when he thought things couldn’t get better, Jean received a note from his organ donor’s family.
“They reached out to me first, and then I wrote them back,” Jean said. “That letter meant so much to me. As soon as I saw who it was from, I just started crying. It’s such a miracle. Someone I don’t even know saved my life.”
Jackson South Medical Center Uses the Latest Robotic Technology in Knee Replacement Procedures
Jackson South Medical Center Uses the Latest Robotic Technology in Knee Replacement Procedures

Jackson South Medical Center is equipped with a new, robotic surgical system that aids in making knee replacement surgery more precise and accurate.
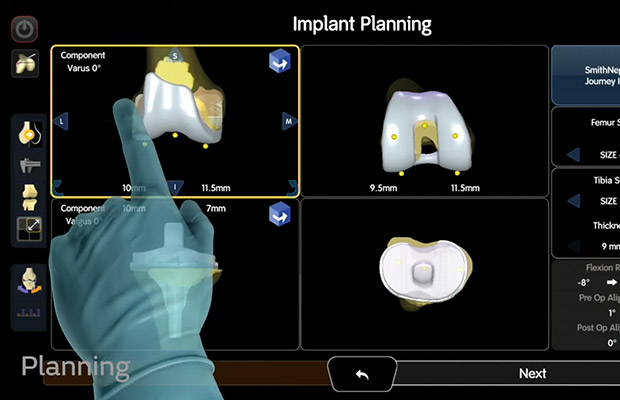
The system provides live, 3-D models that help surgeons plan and perform knee replacement procedures with more precision because it allows them to personalize everything – from the size of the implant components, their fit, and the mobility of a new joint.
Jackson South is the only facility in Miami-Dade and Broward counties with a CORI Surgical System for knee replacement procedures. So far, the Jackson team has performed more than 100 knee replacements using this new technology.
We caught up with Jaime Alberto Carvajal Alba, MD, a UHealth – University of Miami Health System orthopedic surgeon who specializes in this type of robotic surgery at Jackson South. Dr. Carvajal explains how this technology works, who can benefit from this type of procedure, and what patients can expect after knee replacement surgery.
Tell us about the new robotic surgical system and how it works for knee replacement surgery.
The CORI Surgical System is a handheld, semi-automated robotic system. It creates a 3D model live during surgery of the patient’s knee anatomy and allows us to assess the person’s range of motion, stability and better understand how their knee behaves. This provides all the information we need to know to restore the person’s own anatomy and assure a knee replacement is placed in an optimal position.
With this particular technology, we see a live 3D model of the patient’s knee during the surgery, so patients do not need to go for CT scans and other imaging before the procedure, as is sometimes required with other systems.
The live, 3D model also helps us set up the surgical plan and adjust it as needed, and then perform the procedure in a very precise manner. It helps me adjust the size of the components, adjust the tension of the ligaments and, at the end of the procedure, ensure the knee is working as it should. The surgery typically takes about one hour.
When someone has knee pain, what is the process for undergoing a knee replacement?
When a patient comes to us with knee pain, we first assess their symptoms and see what conservative measures they’ve tried first. We always recommend conservative management first, such as physical therapy, oral medications, and sometimes injections to see if we can decrease inflammation and pain.
If these measures do not help or aren’t enough to get the patient back to an adequate quality of life, then we offer surgery. Surgery is an option for almost anyone, as long as they don’t have other serious medical conditions that could make the procedure a risk for them.
Who is a candidate for knee surgery using this new handheld robotic system?
This system works for anyone in need of a knee replacement. Using a robotic system increases the accuracy of implant placement, which leads to optimal outcomes.
What’s the recovery processes like after knee replacement surgery?
At Jackson, we’ve been pioneers of a rapid recovery protocol that gets patients back on their feet and back to living their life as soon as possible.
Two hours after the surgery, we help patients out of bed and back on their feet. A physical therapist will come by with a walker to help them begin putting pressure on the leg.
Our patients go home the same day as surgery, which is nice because people enjoy being back in their homes and recovering in their own bed. We send them home with oral medications to control blood clotting and to manage any pain. In most cases, pain usually diminishes within a few days when the inflammation goes down.
Patients have their first physical therapy session the day after surgery. Our goal is to take the walker away about one-and-a-half to two weeks after surgery. Then, they will use a cane for another week or two, as needed.
Most of our patients generally return to their full activity about four weeks after surgery.
Is there anything else a patient should know before considering a knee replacement surgery?
I highly recommend people seek out a team – with a surgeon and surgical support team – that specializes in knee replacement procedures. At Jackson South, we are a high-volume facility performing hundreds of these procedures each year with an entire surgical team dedicated to this type of surgery. This means we have perfected our procedures down to the tiniest details, ensuring the best experience and outcome for our patients.
For more information or to make an appointment at Jackson Health System for robotic knee replacement surgery, call 305-256-4334.
Cutler Bay Man Back on his Feet After Traumatic Brain Injury
Cutler Bay Man Back on his Feet After Traumatic Brain Injury



In May 2021, Pedro Grillo and his wife were working out when he started to suffer from a severe headache and extreme exhaustion. Grillo, who was confused at his sudden exhaustion, sat on the floor to regain his energy when he lost consciousness.
Gym staff called 911 as Lyannete Soca-Grillo tended to her husband.
Fire rescue rushed Grillo to the emergency department at Jackson South Medical Center, where he was diagnosed with a ruptured arteriovenous malformation (AVM), an abnormal connection between arteries and veins, which causes severe hemorrhaging in the brain.
Due to COVID-19 protocols restricting visitation, Soca-Grillo was not immediately allowed in the hospital, and by the time they allowed her in, her husband was already intubated. The doctors told her he had fallen into a coma, and his condition was quickly worsening. Grillo was transferred to Jackson Memorial Hospital, where Jacques J Morcos, MD, a UHealth – University of Miami Health System neurosurgeon, was on standby to remove the blood in his skull.
“When the doctors told me they had to transfer Pedro, they warned me that he may not survive the ambulance ride to Jackson Memorial,” Soca-Grillo said. “I was terrified. My husband was alone, unconscious, and didn’t have any idea what he was going through.”
At Jackson Memorial, Dr. Morcos and his staff stabilized Grillo and removed the hemorrhage. A few days later, Dr. Morcos performed a craniotomy – a surgery to open the skull – to remove the AVM. He placed a shunt in Grillo’s brain to drain the excess fluid in his skull.
“AVMs are usually present at birth and are typically only detected after they rupture,” Dr. Morcos said. “Brain AVMs, such as Pedro’s, are rare and affect less than one percent of the population. People living with AVMs can live a long and healthy life without it ever rupturing.”
Grillo spent the next four weeks in a coma at Jackson Memorial recovering.
“All those weeks without Pedro were difficult for me,” Soca-Grillo said. “I couldn’t remember the last good memory we had. I could only picture him in the hospital.”
In July, Grillo’s medical team slowly brought him out of his medically-induced coma. He was unable to speak, eat, or walk, and he suffered from short-term memory loss.
“The last thing I remembered was being in the gym,” Grillo said. “I don’t remember waking up in the hospital, and when I first heard about my injury, I just couldn’t believe it.”
The next phase of his recovery consisted of rehabilitation. Grillo and his wife met with physical and occupational therapists from Christine E. Lynn Rehabilitation Center for The Miami Project to Cure Paralysis at UHealth/Jackson Memorial to discuss his recovery plan.
Over the next month, Grillo underwent intense inpatient occupational and physical therapy sessions four times a week, eight hours a day. After his discharge in August, he continued outpatient therapy at Lynn Rehabilitation Center.
“During our therapy sessions with Pedro, we made it clear to him that we were working to help him regain his independence,” said Gemayaret Alvarez, MD, a UHealth physical medicine physician and medical director of neurorehabilitation at Lynn Rehabilitation Center.
Grillo took his therapy seriously – practicing the skills and exercises he learned daily. He knows that the first year post-surgery is the most critical time frame in his recovery, and he hopes to return to his old self.
“When I saw Pedro after his time at rehab, I couldn’t believe how much better he’s gotten,” Dr. Morcos said. “This was a man who was on the brink of death and is now back on his feet and talking, both of which he couldn’t do when I first operated on him.”
In December 2021, Pedro passed his simulated driving assessment at Lynn Rehabilitation Center and accomplished his goal of being able to drive. He now drives himself to and from his rehab visits. His next big milestone is returning to work at CVS Health.
Today, Grillo is able to walk and climb the stairs of his Cutler Bay home without the aid of a walker or cane. Grillo and his wife are excited to finally be together and resume their lives after missing so much time with each other.
“I’m incredibly blessed to be here today, and when I think back to my injury, it almost doesn’t seem real,” Grillo said. “I’m so thankful to the therapist at Lynn Rehab and the doctors at Jackson Memorial for saving my life.”
Mom Looks Forward to Taking Baby Home After Preterm Birth
Mom Looks Forward to Taking Baby Home After Preterm Birth




When Latevia Ward, a third-grade teacher in Miami, went to the hospital in August at 27 weeks pregnant, she knew something wasn’t right. She was recovering from a recent bout of COVID-19 but felt like she was experiencing early signs of labor.
Doctors at the Women’s Hospital at Jackson Memorial Hospital were monitoring her closely because Ward — a mother of 7 — had a history of preterm labor and preeclampsia, which results in dangerously high blood pressure during pregnancy.
Just one year ago, on August 6th, 2020, Ward delivered twins at 27 weeks. The twins, Aidan and Asia, weighed less than two pounds and struggled with many complications. Ward lost both within a matter of months — one-month-old Aidan on Labor Day and four-month-old Asia on Thanksgiving morning.
In 2018, Ward lost another baby girl, Miracle, who was also born prematurely.
With this pregnancy, Ward had been in the hospital several times already due to issues stemming from preeclampsia, which was frustrating because she only had high blood pressure when pregnant. And after losing her previous three babies, she tried to get as healthy as possible.
“You can’t be prepared for it,” Ward said of preeclampsia. “[Before this pregnancy] I had lost weight, was eating right and everything, and wasn’t even on high blood pressure medicine. But as soon as I got pregnant, preeclampsia came back.”
Ward continued to go to the hospital every three days for monitoring. Then, doctors checked her cervix and realized she was dilated, a sign her body was preparing for labor.
Ward was in the hospital on bed rest for seven days, and doctors gave her medications to try to slow or stop the delivery and to prevent complications in the baby if it was born early.
On September 14, Ward went into labor and delivered a baby boy via cesarean section. Aaron weighed 4 pounds. The moment Ward heard him cry, she knew something was different. She never heard her twins cry because as soon as they were born, they needed to be intubated to help them breathe.
“When I heard him cry, I started crying because it was a relief to me,” she said.
Aaron was whisked away to the Neonatal Intensive Care Unit (NICU) at Holtz Children’s Hospital, the largest Level III NICU in the region that can provide care for the sickest and smallest babies.
Within four days, Aaron was off the CPAP breathing machine, but Ward was still nervous. She feared something would go wrong.
“I was afraid about everything,” she said. “I was so sad all over again thinking about my other babies.”
The nurses in the NICU, especially those who know her from the previous year, have reassured her each day that Aaron is doing well and getting stronger. He is tolerating food and is learning to suck to be able to eat from a bottle. He is now 8 weeks old, weighing more than 5 pounds.
“He’s alert and doing better,” Ward said. “I’m able to relax a little. But I still have some bad days, [especially since] November is when I lost Asia.”
Despite her understandable fears after her unimaginable loss, Ward has faith that Aaron will pull through.
“You just have to stay strong. I’m spiritual, and I read my Bible to stay positive, and I have positive friends around me,” Ward said.
Ward’s original due date was November 25, and doctors believed he would be ready to go home by then, but on Friday, November 12, Ward received the much-awaited that her baby boy was finally coming home.
Ward is looking forward to that day.
“I’m thankful to God that my son has finally come home and now we get to spend time together as a family,” She said.
A Mother’s Unconditional Love Gives Son a Fighting Chance to Receive a Life-saving Kidney Transplant
A Mother’s Unconditional Love Gives Son a Fighting Chance to Receive a Life-saving Kidney Transplant





When Araceli Cantero Obregón was seven months pregnant, doctors in Nicaragua told her that her son Edgard Sequeira would have hydrocephalus, a condition in which excess cerebrospinal fluid (CSF) builds up within the ventricles of the brain. She was also advised that they identified spina bifida, which occurs when a baby’s spinal cord fails to develop properly in the womb.
Despite the heartbreaking news, Obregón was not going to give up on her first-born son, who she welcomed into the world on September 6, 2007. By the time Edgard turned one, he had undergone surgery for both conditions. The procedures allowed the family a sense of normalcy for a few years, but the young boy continued to face medical setbacks and personal hardships.
Throughout his childhood, Edgard was not developing physically or cognitively. He also was experiencing complications with his bladder and kidneys. Furthermore, Obregon began noticing her son was lacking energy. He was isolated from his friends and had occasional seizures.
In 2016, pediatricians in Nicaragua ran tests and gave Obregon frightening news — her son was diagnosed with chronic kidney disease (CKD) and would need to start dialysis immediately. Edgard was also suffering from high blood pressure. The diagnosis was an all too familiar red flag for Obregón, who had lost her husband to CKD two years prior.
“It was traumatic to hear my son was suffering from the same disease that took my husband,” Obregón said. “My whole world was falling apart.”
After years of attempts with no sustainable treatment, Obregón desperately sought the care of pediatric nephrologists at Holtz Children’s Hospital, leaving Nicaragua for the U.S. in February 2020.
When Edgard arrived at Holtz Children’s, he was malnourished, weighing 50 pounds at 12 years old. After a thorough examination, his team of nephrologists determined he needed intervention in urology, nutrition, and blood pressure care before he could be listed on the national transplant waiting list. He would also need to continue receiving dialysis four times a week while being monitored by the pediatric transplant team at the Miami Transplant Institute (MTI).
Due to the COVID-19 pandemic, the family was also faced with the decision of having to stay in Miami long-term. For Edgard to have a fighting chance, Obregón knew the best decision was to stay in South Florida and make sure her son completed his treatments.
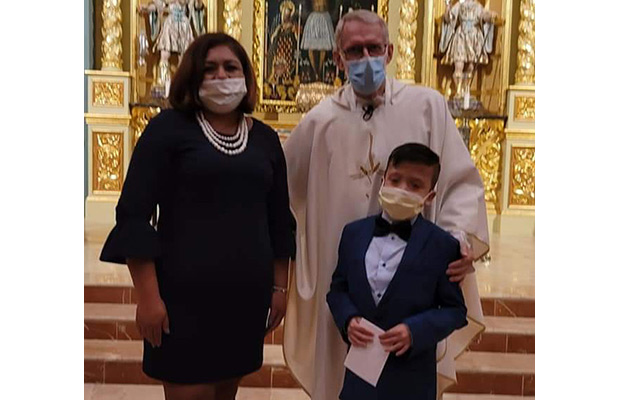
Thanks to the help and financial support of family, friends, and Miami’s Corpus Christi Catholic Church, Edgar and Obregon were able to stay in the U.S. and continue with Edgar’s care.
Over time, Edgard, now 14, had breakthroughs in his health, and last October, he was listed on the national transplant list. Five days after her son was listed, Obregón received the call from MTI that they were ready to perform the life-saving procedure.
The successful kidney transplant was led by Mahmoud Morsi, MD, and a multidisciplinary team at Holtz Children’s.
“I am eternally grateful to everyone, the social workers, the nurses, the nephrologists, the Holtz team, the MTI team, and so many others who have become a part of our family,” Obregón said. “There is no way to repay them for giving my son a chance to have a better quality of life.”
For the care team, miracle stories like these also remind them of their life’s calling as medical professionals.
“It’s a gift for them, and it’s a gift for us,” said UHealth pediatric nephrologist Jayanthi Chandar, MD. “It gives us a sense of fulfillment and happiness to see our patients thrive and witness extraordinary changes in their mental, emotional, and physical state.”
After 123 Days in the NICU, Baby is Reunited with his Parents
After 123 Days in the NICU, Baby is Reunited with his Parents


When Patricia Fusco and Katrina Wegmann were in high school, Patricia shared that she would not be able to carry and birth her own children. Unbeknownst to Patricia, Katrina decided then that if she was able to when the time came, she would be a surrogate for her friend.
Little did they know that more than 20 years later, not only would they still be close friends, but their husbands would also be best friends. And when Patricia and her husband, Andrew, had trouble finding a surrogate, Katrina stepped up.
Katrina, who already had two children of her own, expected it would be “another easy pregnancy and it would be able to make them a family.”
The pregnancy turned out to be anything but easy. Twelve weeks into her pregnancy, Katrina’s blood pressure was high — something she’d never experienced before, causing the pregnancy to be considered “high risk.”
Turning to Jackson for High-Risk Care
As the pregnancy progressed, Patricia, a senior specialist for community outreach and events at Jackson Health System, asked Katrina to consider meeting with the Maternal Fetal Medicine team at Jackson Health System. Every year at work, Patricia plans multiple events, including the NICU reunion, where babies who were saved and cared for at the Holtz Children’s Hospital Neonatal Intensive Care Unit (NICU) are reunited with their medical teams.
“I know that Jackson treats over 50 percent of South Florida’s high-risk pregnancies and that the Holtz Children’s Hospital NICU is one of the largest and best in the nation,” she said. “Working at Jackson, I hear the miracle stories all the time. But you never think you’re going to be one of those miracle stories.”
Katrina and Patricia immediately felt comfortable and confident in the Jackson team. They were followed by Jackson Medical Group physicians, Dana L. Homer III, MD, FACOG, an OB/GYN, and Felipe Tudela, MD, FACOG, an OB/GYN and maternal fetal medicine specialist.
Patricia called Tudela “a gift to his profession.”
“He’s probably the best doctor I have ever had the pleasure of meeting,” she said. “Everyone on the team invests themselves wholeheartedly in each patient’s case.”
When Katrina was 23 weeks pregnant, she suffered from terrible headaches, and her blood pressure was extremely high. She was admitted to the hospital and told she would need to remain there on bed rest to try to prevent an early delivery. That meant a possible two-to-three-month hospital stay – a stressful complication since she had two small children at home. Later they would confirm she had preeclampsia, a potentially dangerous pregnancy complication associated with high blood pressure.
A Difficult Choice
Two weeks later, a routine ultrasound showed that the baby was not growing and there was concern with the placenta, which was no longer providing critical nutrition to the baby. Dr. Tudela told them to consider delivering the baby early because he did not know if the baby would survive otherwise. Patricia, Katrina, and their husbands came together to make the difficult decision.
“That was a terrifying day for us, probably one of the most emotional days,” Patricia said. “Ultimately, we trusted the Jackson NICU enough that we preferred to deliver him then, rather than seeing what could happen if we tried to keep him in utero.”
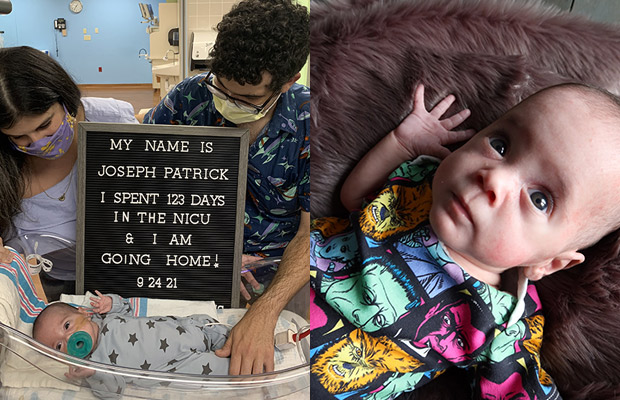
On May 27, 2021, at 25 weeks and five days gestation, Joseph Patrick, nicknamed JP, was born weighing just 1 pound 4 ounces. Quickly, doctors told the Fuscos that they made the right choice as there was no more amniotic fluid in the sac, and the baby would not likely have survived if they had waited.
As soon as the Fuscos saw their baby in the NICU, they felt more at ease.
“When we saw him, I thought, ‘they’ve got this,” Patricia said. “Once he was stable in the NICU, things began to feel safe. And every step of the way from that day forward, the doctors, nurses, therapists, everyone at every level always kept us abreast of what was going on.”
The NICU Village
JP thankfully had no brain bleeds and a fairly smooth ride in the NICU, with some breathing complications and an unknown infection during his stay. He remained in the NICU for 123 days.
“They say it takes a village [to care for a child], and I can wholeheartedly say there is no better village than the NICU village at Holtz Children’s,” Patricia said.
During JP’s stay, Patricia and Andrew said they were a part of every conversation regarding his care and the nurses became their friends, confidants, and teachers.
In addition to the expert and compassionate care that both Katrina and JP received, Patricia said she is grateful that everyone at Jackson treated their uncommon situation as if it were an everyday occurrence.
“We had a unique situation because we were high-risk. It was also unique because it was a surrogacy, and we were two friends going through this together,” Patricia said. “We know that our situation is not common. It definitely is not something they see every day. But every single physician, every single healthcare worker, never batted an eye at us. Everyone treated the experience with understanding and compassion. I don’t know if that would have been the case at another hospital.”
In September, after a nearly four-month NICU stay, JP was able to go home.
“It was a relief to finally be able to walk out of those doors with our son,” Patricia said. “It felt like an accomplishment.”
A Special Bond
JP continues to grow and thrive but is closely monitored by doctors and specialists to make sure he’s developing and that no more complications arise. Patricia and Andrew are now enjoying what they call a more “normal” stage of parenting.
“We’ve already seen him grow from a fragile 1-pound infant to a robust, beautiful baby boy,” Andrew said. “Now I’m looking forward to watching him hit those milestones, not only growth and developmental milestones but the little kid moments that define a childhood.”
And Katrina is happy that she will be there to witness it all. While they still need to be careful about visits due to the pandemic, the families are closer than ever.
“I talk to my kids about JP all the time, and they can’t wait to spend time with him. I look forward to them growing up together,” she said.
The experience “intertwined” the families forever, Patricia said.
“We are eternally grateful to her,” she said. “There are no words or ways we could ever adequately repay or thank her for what she has given us.”
Baby Reunites with Parents after Months in the NICU
Baby Reunites with Parents after Months in the NICU

In December 2020, Daniel Furlong, a former urology resident at Jackson Memorial Hospital, and his wife, Sarah, were packing for their babymoon trip – four months before the expected arrival of their first child – when suddenly, Sarah began to experience uterine cramps.
The couple immediately rushed to The Women’s Hospital at Jackson Memorial, where doctors determined Sarah was in preterm labor. She remained hospitalized for observation, but the baby just couldn’t wait.
On December 30, 2020, with the help of Rachel Franklyn, MD, Jackson Medical Group associate medical director of obstetrics and gynecology, Sarah gave birth to a baby boy at nearly 25 weeks. Ryder, who weighed just 1 pound, 10 ounces, was immediately rushed to the neonatal intensive care unit (NICU) at Holtz Children’s Hospital. He remained intubated in the NICU for two months and had to overcome several medical setbacks, including pneumonia and brain bleeds, which caused him to have several seizures.
Ryder was also diagnosed with a condition called patent ductus arteriosus (PDA), an opening between the two major blood vessels leading from the heart that normally closes shortly after birth. He underwent a PDA ligation procedure, performed by Eduardo Alfonso Perez, MD, a University of Miami Health System pediatric surgeon, to correct the birth defect.
“He had to overcome so many medical challenges in the NICU that his medical team began calling him ‘Ryder the fighter’,” his father, Dr. Furlong, recalled.
When Dr. Furlong wasn’t tending to his patients, he was at his son’s bedside. Due to COVID-19 visitation restrictions, he and his wife took turns visiting Ryder.
“As a physician, I struggled with knowing too much and trying to relay that information to my wife without scaring her while being honest with her about Ryder’s progress,” Dr. Furlong said.
Last May, after spending 125 days in the NICU, Ryder was finally able to go home. The Furlong’s family and friends had anxiously awaited for this moment to come.
“Having Ryder as a patient was a journey for my staff and me,” said Dianne Bennett, ARNP, director of patient care services at Holtz Children’s. “Seeing him finally reunited with his parents after all he had gone through was such a heartwarming moment.”
Dr. Furlong and his wife are happy to be settling in with their son.
“Hearing Ryder cry at home was such a relieving moment,” Dr. Furlong said. “My wife and I had waited months to finally be with our son. We were so overjoyed to have him with us.”
Ryder will continue to visit various specialists to make sure he’s progressing and meeting important developmental milestones.
“As a member of the Jackson family, it was encouraging to know that my son was truly in the best care possible,” Dr. Furlong said. “My wife and I are so appreciative and thankful to everyone who took care of Ryder, including all of the doctors, nurses, therapists, and ancillary staff who treated and loved him as their own child.”
New York Man Brought to Jackson Health System for Life-saving Neurosurgery
New York Man Brought to Jackson Health System for Life-saving Neurosurgery

In May 2021, Zac Yezzi found himself in a life-threatening situation after he suffered a stroke.
Yezzi and his fiancé were in St. Barts planning their wedding, when one morning, the 30-year-old began developing a splitting headache that lasted throughout the day. He then lost vision in his right eye, followed by function in his right arm and leg. Somehow, he managed to drag himself to the bathroom and splashed himself with water.
“I was not aware of how traumatic my injury was then, but I knew something was terribly wrong,” Yezzi said. “I asked my fiancé to dial emergency services and request an ambulance.”
Yezzi was rushed to a nearby hospital, where a CT scan revealed that he had a large, eight-centimeter hemorrhage on the left side of his brain, which controls speech. The average hemorrhage is measured in millimeters.
With no neurologist on staff at the hospital in St. Barts, Yezzi was flown to a larger hospital on the nearby island of Guadeloupe. He arrived alone, afraid, and in agonizing pain, unable to communicate with his medical team, who only spoke French.
In Guadeloupe, doctors performed additional tests on Yezzi’s brain, and the results revealed an arteriovenous malformation (AVM) –an abnormal connection between arteries and veins, which would require complex neurosurgery that the hospital was not equipped to perform.
The AVM was determined to be the cause of Yezzi’s initial stroke and hemorrhaging.
While this was happening, Yezzi’s family had contacted the Bee Foundation, an organization that raises awareness about brain aneurysms and hemorrhages. The foundation played a crucial role in getting him transferred by connecting his family with a French-speaking neurosurgeon to communicate with the medical staff in Guadeloupe.
After two days, Yezzi was medically evacuated to Jackson Memorial Hospital. He was accompanied by his fiancé and his father, who were finally able to arrive in Guadeloupe despite multiple flight complications.
“The days leading up to my medevac were two of the longest days of my life,” Yezzi said. “During the flight to Miami, the pressurized cabin was causing me indescribable levels of pain, but I was just relieved to have my fiancé at my side.”
Upon arriving at Jackson Memorial, Yezzi was immediately placed in the neurointensive care unit, where he and his family met with Robert M. Starke, M.D., a University of Miami Health System neurosurgeon and neuroradiologist.
Dr. Starke walked Yezzi and his family through his diagnosis and recommended surgical embolization of the aneurysm and AVM and a craniotomy to remove the aneurysm as the best course of action if they wanted to prevent any recurring brain bleeds.
“Zac should consider himself fortunate,” Dr. Starke said. “Normally, a brain bleed as big as his has the potential to squash the brain, which could lead to death or severe long-term damage.”
After considering his choices, Yezzi elected to undergo surgery.
“I owe everything in my life to Dr. Starke! He and his team saved my life,” Yezzi said. “He’s an incredible surgeon. I’m so lucky to have been transferred to Jackson Memorial.”
Yezzi and his fiancé are back home in New York City, where he’s resumed work. He has made a full recovery, regained his sight, as well as the function in his right arm and leg.
He’s working on promoting awareness and the importance of early detection of brain aneurysms and AVMs to prevent others from having to go through a similar injury.
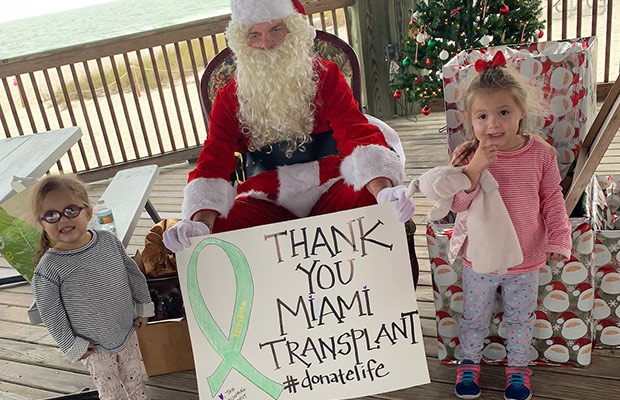
Naples Twin Celebrating Her Third Transplant Anniversary after Rare Diagnosis of Alagille Syndrome
Naples Twin Celebrating Her Third Transplant Anniversary after Rare Diagnosis of Alagille Syndrome







For first-time parents, JoAnna and Kris Palinchak, having twin girls was a dream come true. But three months after delivering healthy twin girls, the new parents noticed that one of their daughters, Ella, was developing differently than her sister, Lacy.
Ella had developed jaundice, a liver condition that causes yellowing of a newborn baby’s skin and eyes. She required immediate medical attention and was taken to a hospital near their home in Naples. Doctors there conducted exploratory surgery and performed a liver biopsy.
Initially, doctors suspected Ella had biliary atresia, a rare and genetic life-threatening disease that affects the bile ducts in the liver of infants. The Palinchaks turned to a trusted gastrointestinal doctor who advised them to have Ella evaluated by the Miami Transplant Institute (MTI), an affiliation between Jackson Health System and UHealth – University of Miami Health System.
Due to their global expertise in complex cases, the medical team at MTI discovered that Ella’s jaundice had manifested into Alagille syndrome, a condition in which bile builds up in the liver because there are too few bile ducts to drain it.
“Alagille syndrome is a rare genetic condition in early childhood in which many organs may be involved, including the liver, heart, brain, kidneys, bones, eyes, and face,” said Tamir Miloh, MD, medical director of MTI’s pediatric transplant hepatology unit. “Ella had developed progressive jaundice, intractable itching, poor sleeping patterns, and stunted growth.”
While normally non-threatening, her condition was causing early-onset liver failure. Though there is currently no cure for the condition, there are ongoing studies at some children’s hospitals on early diagnosis and new innovative medical interventions aimed at improving outcomes and quality of life in these children. Holtz Children’s Hospital at the University of Miami/Jackson Memorial Medical Center is among the hospitals with experience treating children with Ella’s condition.
After meeting with doctors at the Miami Transplant Institute and Holtz Children’s, Ella’s parents were told the best treatment for their daughter would be a liver transplant.
Although the family was scared after receiving the news, they had confidence in Ella’s medical team and quickly bonded with them — especially Kati Garcia, her assigned nurse and transplant coordinator, who had been with the family every step of the way.
“We were afraid, but Kati was very helpful in helping us understand everything that was happening,” Ella’s mom said.
On December 16, 2016 -one day before her first birthday – Ella was listed on the national transplant waiting list.
The Palinkchaks remained hopeful, but the developmental delays of their baby girl began to discourage them. While Lacy began walking at nine months, it took Ella 24 months.
The loving parents would spend the next two years traveling between their home in Naples and Holtz Children’s.
“She was followed by a transplant and heart teams to optimize her nutritional status while we waited for an appropriate donor,” said Dr. Miloh. “Before safely undergoing transplant surgery, she needed intense nutrition support including fat-soluble vitamins and targeted therapy for severe debilitating itching associated with Alagille.”
On March 8, 2018, Ella’s parents were notified that a donor liver was found for their daughter. They quickly packed their bags and drove to Miami.
As the medical team prepared Ella for transplant surgery, the peaceful look on her face gave the worried parents a sense of security that everything was going to be fine. The following morning, Ella underwent a successful liver transplant led by Akin Tekin, MD, UHealth’s liver, intestinal and multivisceral surgeon, and a multidisciplinary pediatric team at Holtz Children’s.
The surgery was a success. And when the Palinchaks got to see their daughter in the pediatric intensive care unit, they were met with an unexpected surprise: Ella’s nurses had brushed and styled her hair.
“We were in the right place, with the right people,” her mother said. “Within two weeks, Ella was discharged, and ever since then, our baby girl started thriving.”
To honor the donor family, a garden with beautiful flowers was planted on the Palinchaks front lawn For Ella and other children who are battling this condition, the Palinchak family hosts an annual fundraiser in their community to raise awareness of Alagille syndrome.
“The family’s selfless act of organ donation during a moment of sadness forever changed our family,” said JoAnna Palinchak. “We have cried sorrowful tears for them and prayed for them. When our daughter is old enough to understand the path of her life, we hope that the ‘person’ at the center of her story can be identified as her lifesaving superhero.”
Now age 5, Ella visits MTI twice a year for check-ups. She’s happy, healthy, and loves spending time with her twin sister.
“Her beautiful scars tell an amazing story that we will never forget,” JoAnna said. “No words are enough to show appreciation and gratitude for all that was done to change Ella’s life. Every single day of her life is better because of the medical team at MTI.”
Sickle Cell Disease + COVID: The Importance of Getting Vaccinated
Sickle Cell Disease + COVID: The Importance of Getting Vaccinated



While 28-year-old Keyondra Smart knew at a young age that she suffered from sickle cell disease (SCD), she didn’t fully understand the effects of the illness until four years ago when she was hospitalized at Jackson Memorial Hospital with acute chest syndrome and double pneumonia, which occurs when the infection affects both lungs.
Sickle cell disease is a group of hereditary red blood cell disorders that causes the cells that carry oxygen around the body to become hard, sticky, and c-shaped like a sickle. The cells tend to die early, leading to a shortage of oxygenated blood cells. The disease can also put a patient at a higher risk of developing infections.
The Center for Disease Control estimates that more than 100,000 Americans suffer from SCD, and 1 in 13 Black or African American babies is born with sickle cell trait.
After a month’s stay at Jackson Memorial, Keyondra fell into a deep depression. She had to relearn how to walk and was struggling with the reality of living with the effects of SCD.
“I was on my deathbed and in the intensive care unit for two weeks,” Smart said. “I had never experienced so much pain before. I was mentally, physically, and emotionally exhausted.”
Slowly, Smart came to terms with the disease and began learning about ways to manage her ongoing pain and symptoms.
She returned to school and was determined to graduate despite days when she did not feel well following her treatment.
A few years passed, and as Smart’s life seemed to be getting better, the COVID-19 pandemic hit.
“My anxiety came back because I was so scared of the virus,” she said. “I already have a weak immune system, and this was something I could die from.”
Sickle Cell and COVID
Thomas Harrington, MD, and Maya Bloomberg, MSN, APRN, are the adult sickle cell providers in the Division of Hematology/Oncology at Jackson Memorial. They explained that patients living with sickle cell are at a greater risk of contracting COVID-19. SCD patients who get sick with the virus experience higher rates of hospitalizations and complications, along with worsening sickle cell pain.
Additionally, studies performed before COVID vaccinations were available and the spread of the Delta variant also showed racial disparities in terms of life expectancy due to the virus.
“While life expectancy dropped for all groups, it has been worse for the Black community,” Bloomberg said. “Overall life expectancy dropped by one year for Caucasians and two years for the Black population.”
One study published via PLOS ONE showed that the difference in life expectancy was due in large part to increased exposure at work and access to personal protective equipment.
COVID-19 Vaccine
Faced with the discouraging disparities and risks to patients with sickle cell, Dr. Harrington and Bloomberg are encouraging their patients and the community to get vaccinated.
“You need to put the relative risks in perspective,” Bloomberg said. “The COVID-19 virus is very unpredictable, especially the latest Delta variant. People assume that only older people with health conditions are getting sick and dying, but more and more we’re seeing younger people in the hospital with severe COVID cases.”
If people are worried about the vaccine or have concerns, she encourages them to turn to speak with their doctor.
Keyondra chose to get vaccinated after speaking with Dr. Harrington, who is one of the few experts in sickle cell care in South Florida.
“I know people are scared because there’s a lot of information out there, and they might think it’s a setup, but you should talk to your doctor about any concerns you might have,” Smart said. “I highly recommend other SCD patients get vaccinated, too. We’re already fighting one disease. Who wants to fight two?”